| E-mail this page to a friend | Tell me when this page is updated |
Conducted
at Le Meridian Hotel, Dubai on 2nd Jan 2001.
Moderator:
Dr.S.M.S.Pillai, Dubai
Editor:
Dr.V.S.Hanish Babu, Ajman
Contents:
vDefinition,
Incidence andPrevalence
vClinical
Features and Complications
vTopical
Therapy Other Than Steroids
vOther
Immunosuppressive Therapy
vDefinition,
Incidence and Prevalence
Contributed
by Dr.S.C.Bose, Sharjah
Introduction:
Psoriasis derives its name from the Greek word for 'itch'. It is a comparatively
easier skin disease to diagnose but very difficult to treat causing frustration
to patient and clinician alike.
Definition:
Psoriasis is a common, chronic and non-infectious skin disease characterized
by well defined erythematous slightly raised plaques and papules with silvery
scales and typical extensor distribution
Incidence
and Prevalence:
Psoriasis is universal in occurence. Genetic and environmental factors
greatly influence the clinical development of the disease. Occurence varies
from 0.1% to 3 % in different parts of the world.
Americas:
1-2 %. Rare in American blacks and absent in Red Indians.
South
America: 0.97%
Germany:
1.3%
Great
Britain: 1.6%
Denmark:
1.7%
Sweden-2.3%
West
Africa-Rare
Japan-Low
Eskimos:
Very Low
No
studies have been done in general population in India, but a study of patients
attending clinics and hospitals showed a prevalence of 0.8% to 5.6%.
Age
of onset:
Even though it can appear at birth as well as very old age, the most common
onset is in 2nd to 4th decades of life.
Familial
Occurrence:
Approximately 1/3rd of the patients with psoriasis has a relative similarly
afflicted.
Sex:
Occurs with almost equal frequency in males and females, but a slightly
higher prevalence noticed in males.
Contributed
by Dr.R.Soman, Dubai
Genetic
Predisposition:
The evidence that psoriasis may be inherited is based on population surveys
and family analysis. Controversy exists on the mode of transmission. More
evidence is in favour of single gene autosomal dominant inheritance with
reduced penetrance.
The
incidence of psoriasis in siblings appears to be as high as 50% when both
parents are affected.
HLA
Systems:
The relationship of psoriasis to HLA system was studied by many researchers.
Many have confirmed association with B13, B17 and CW6. In GPP strong association
with HLA B8 and in GPP association with B27 was found.
Provocative
and exacerbating Factors:See
below.
Endocrine
Factors:
Peaks of psoriasis has been reported during puberty and menopause. Psoriasis
remains unaltered in about 40% of pregnancies, improved in 40% and worsened
in 15 %. GPP may be provoked by pregnancy and may get exacerbated premenstrually
and with high dose estrogen therapy.
Metabolic
Factors:
Hypocalcaemia following parathyroidectomy and dialysis has precipitated
psoriasis.
AIDS:
The prognosis of Psoriasis in AIDS patients and AIDS in psoriatic patients
appears to be poor due to the decrease in T helper cells.
Also
see Pathogenesis, immunology, biochemical aspects and provocative factors
below for a full review of aetiopathogenesis of psoriasis.
 |
Contributed
by Dr.T.C.Satish, Dubai
It
is a complex interaction between alteredkeratinocytic
proliferation & differentiation, inflammation & immune dysregulation.
The
earliest
changes are vascular. There is swelling & intercellular widening
of endothelial cells followed by deregulation of mast cells around post-capillary
venules. Hours later activated macrophages appear in the lower epidermis
where there is loss of desmosome tonofilament complexes. Finally lymphocytes
& neutrophils appear.
Electron
Microscopic studies shows psoriatic keratinocytes have significant abnormalities.
Tonofilaments are decreased in number and diameter and lack normal aggregation.
Keratohyaline granules are decreased in size and number. The cornified
cells retain organelles and nucleus as parakeratotic cells. The basal keratinocytes
show cytoplasmic processes protruding into dermis through gaps in the basal
lamina and they correlate with disease activity. The intercellular spaces
between all epidermal cells are widened because of deficiency in the glycoprotein
rich cell surface coat. The spongiform pustule of Kogoj, one of the most
characteristic features of psoriasis is located in the uppermost portion
of spinous and granular layers. Here neutrophils lie intercellular in a
multilocular pustule in which sponge like network is composed of degenerated
and flattened keratinocytes. The capillary loops in dermal papillae in
psoriasis show wider lumen, bridged fenestrations & gaps between endothelial
cells, extravasation of RBCs and inflammatory cells & thickened basement
membrane. They may be due to deposition of amorphous substances & accumulation
of collagen fibrils in the BMZ.
EPIDERMAL
CELL KINETICS
The
rate of epidermal cell replication is markedly increased as suggested by
the higher number of basal and suprabasal mitotic figures. The mitotic
activity varies in different lesions & even within the same lesion.
It correlates with degree of parakeratosis.Early investigations suggested
that the transit time of cells from basal cell layer to uppermost row is
shortened to 7 days in psoriasis from 53 days in normal epidermis. Further
investigations showed the germinative cell cycle shortened from 311 to
36 hrs i.e. 8 fold faster proliferation in psoriasis, doubling of proliferative
cell proliferation in psoriasis from 27000 to 52000 cells/sq mm of epidermal
surface area, 100% of germinative cells of epidermis enter growth fraction
instead of only 60% for normal subjects. However another study showed that
the germinative cell cycle time in normal epidermis is 200 hrs while in
psoriasis it is only 2 fold faster i.e. 100 hrs. The source of cycling
cells in suprabasal layers is not yet well defined. It could be expanded
population of basal keratinocytes or could be recruited from transit amplifying
cells (TAC) which are suprabasal keratinocytes committed to terminal differentiation
that undergo rounds of amplifying divisions above basal layer. Keratin
studies suggest TAC since they express K1/K10 & K6/K16 keratins and
not K5/k14 as basal keratinocytes do.
KERATINOCYTE
DIFFERENTIATION
Keratinocytes
undergo a process of differentiation as they migrate upward through the
epidermis from basal layer to cornified layer when several structural proteins
are synthesized. One such protein family is keratins, which are intermediate
filaments, found in the cytoplasm of all epithelial cells. Studies show
that in normal epidermis K5/K14 are expressed in basal keratinocytes and
K1/K10 are expressed in suprabasal keratinocytes. Involucrin, one of the
major precursor proteins of cornified cell envelope are detected higher
in granular & cornified layers. In psoriatic skin basal keratinocytes
continue to expressK5/K14. However keratins K1/K10 are replaced by so called
hyper proliferation associated keratins K5/K16.Also involucrin expressed
prematurely in lower suprabasal layers. K17 also found in upper suprabasal
keratinocytes while normally they are found in deep outer root sheath of
hair follicle.
Immuno
pathological factors also play a very important role in the pathogenesis
of psoriasis.
Contributed
by Mammen Jacob, Sharjah
Contributed
by Dr.Lilly Jose,Sharjah
Since
the aetiopathogenesis of psoriasis is still not well established, there
are several postulations.
The
biochemical aspects of psoriasis are mainly related to the arachidonic
acid metabolism. The release of arachidonic acid is increased by the enhanced
activity of phospholipase A2.The cycloxygenase pathway is inhibited in
psoriatic skin so this acid is diverted to the lipoxygenase pathway leading
to increase in concentration of many human peripheral leucocytes attractants
like leukotrene B4, eicosatetraenoic acid, interleukines, peptides, platelet
activating factors etc.
Another
important factor implicated is the complement C5a (des arg) derivative.
This is produced due to compliment activation by complexes formed between
stratum corneum antigens and antistratum corneum antibodies.
All
the above factors as well as increase in the epidermal growth factor, increase
in IL6 and LTB4 etc increases the mitogenic potential. The alterations
in the cyclic AMP, cGMP ratio also contributes to this. CGMP is increased
and cAMP is decreased in psoriatic skin.
There
are controversial reports about a decrease in Protein Kinase C, metabolite
of phosphotidyl inositol. Protein Kinase C deficiency leads to increase
in mitosis.
Calcium
andits binding protein calmodulin
modulate growth and differentiation of cells. Increase in calcium binding
protein is seen in psoriatic skin leading to increase in epidermal proliferation
Ornithidine
decarboxylase is the rate-limiting enzyme in the synthesis of polyamines
(spermidine, spermine and putrescine), which in turn increase DNA synthesis
and cell proliferation. Some reports are showing an enhanced production
of polyamines in the causation of increased epidermal proliferation.
Most
of the changes are not specific for psoriasis. To some extent these alterations
are seen in contact dermatitis, atopic dermatitis etc also.
Contributed
by Dr.Hanish Babu, Ajman
Psoriasis
is marked by periods of remissions and exacerbations. Remissions usually
last a few weeks to many years. Both local and systemic provocation factors
bring in exacerbations.
Local
Factors: Local
injury to the skin produces psoriatic lesions, the well-known Koebner Phenomenon.
Trauma
involving the papillary dermis could be physical, chemical, mechanical,
allergic or burns, drug eruptions, dermatitis, lichen planus, miliaria,
herpes zoster, chickenpox etc. Koebner phenomenon occurs usually within
7-14 days (ranging from 3 days to 3 weeks)
Seasonal
variations: In
most patients, psoriasis worsens during cold weather. High humidity is
usually beneficial, whereas sunlight worsens in some but improves in many.
Pregnancy:In
most cases pregnancy induces remissions, though raised levels of progesterone
in the latter half of pregnancy can precipitate generalized pustular psoriasis
in some.
Emotional
Stress: Psoriasis
is well known to be induced, exacerbated, or sustained due to emotional
stress. The mechanism is not yet well understood, but neuropsychoimmunological
mechanisms are hypothesized. The disease itself could produce a reactive
depression, which could further exacerbate the disease.
Infections:Streptococcal
URTI has been shown to exacerbate existing psoriasis and precipitate an
attack of acute guttate psoriasis mainly in children. Koebner phenomenon
also produces psoriatic lesions in certain bacterial, fungal and mycotic
skin infections. Other hidden infective foci from sinus, tonsil, gall bladder,
appendix, urogenital tract, and oral cavity also may be the cause for exacerbation
of psoriasis in certain individuals.
Drugs:Many
drugs are known to precipitate or exacerbate psoriasis.
Beta-blockers
like propranalol, practalol, and metapralol may induce or exacerbate psoriatic
eruption by depressing the cyclic AMP levels. The eruption usually disappears
within 2 to 6 weeks of cessation of the drugs.
Almost
all NSAIDS affect psoriasis adversely. Anti depressants like lithium compounds
and Trazodone may precipitate generalized pustular psoriasis.
Too
rapid withdrawal of corticosteroid therapy may precipitate pustular or
erythrodermic exacerbations of psoriasis.
Alcoholic
beverages affect psoriasis adversely.
Chloroquine,
clonidine, iodides, glibenclamide, and tetracycline are a few other drugs
known to exacerbate psoriasis.
Very
harsh or overenthusiastic topical therapy is also a culprit.
The
role of food visa viz psoriasis is controversial. Red meats are generally
considered to exacerbate psoriasis. A few shellfish may stimulate an acute
exacerbation while, as a whole fish is considered beneficial in psoriasis.
Fish oils containing essential fatty acids have been found to be effective
in many patients, though conclusive evidence is still awaited.
Contributed
by Dr.George Jacob, Ras al Khaima
 |
In
the EPIDERMIS, the characteristic changes consist of acanthosis and elongation
of the rete ridges, a reduced or absent granular layer, parakertosis, oedema
of the papillae and thinning of the super papillary plate, and the presence
of micro pustules in the upper epidermis. The early changes: The
first histopathological change is invasion of the epidermis by neutrophil
polymorphs (and maybe a small micro abscess). The changes in established
psoriasis:are essentially epidermal.
The horny layer shows considerable hyper & parakeratosis, often alternating.
The granular layer is reduced or absent in active lesions.
The
rete ridges are greatly elongated & often clubbed. They are separated
by oedematous papillae, also club shaped, above which the spinous layer
is thinned. Mitotic activity is the basal and suprabasal cells are greatly
increased. Cellular invasion takes place, particularly in the suprapapillary
region to form the Munro 'micro abscess' which are extruded in the
horny layer or they may collect in disintegrated malphigian cells, the
cytoplasm of which had been lysed to form the multilocular or spongiform
pustule of
Kogoj.
In
the DERMIS the main changes consist of papillary oedema, dilatation and
tortuosity of the papillary capillaries and a mild to moderate infiltrate
of lymphocytes with occasional histiocytes.
vClinical
Features and Complications
Contributed
by Dr.Balachandran,Dubai
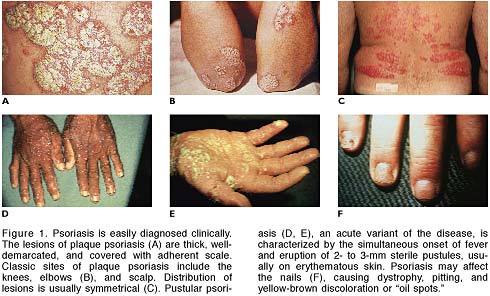
Development
of erythematous well-defined, dry, scaly papules and plaques of varying
sizes characterize psoriasis.
The scales are abundant, loose, dry (sometimes greasy) and silvery white.
On scrapping, characteristic adherence of scales can be seen as if one
scratches on a wax candle. When the scales are completely scrapped of,
a moist, pinpoint bleeding surface is seen. Development of isomorphic lesions
at the site of local trauma is more common during the acute or eruptive
stage (Koebner phenomenon).
In
some patients, raindrop like erythematous papules erupt abruptly with a
bilaterally symmetrical distribution. This type of guttate lesions may
also occur in patients with chronic plaque psoriasis when they are exacerbated
or become eruptive. Chronic plaque psoriasis is common type. If palm sized
lesions predominate, it is called psoriasis geographical and if coin shaped
lesions predominate, it is called nummular psoriasis.
Sudden
withdrawal of corticosteroids or application of irritants can cause erythema
and scaling. This condition is called exfoliative psoriasis. Patients may
have hyperpyrexia, hypoalbuminaemia, eneteropathy and generalized lymphadenopathy.
Sometimes
over treatment with tar, anthralene or potent steroids or by systemic therapy
with progesterone or corticosteroids may lead to development of superficial
pustules on the surface. It is called pustular psoriasis. This may be localized
or generalized. Impetigo herpetiformis that occurs in last trimester of
pregnancy is considered to be a variant of generalized pustular psoriasis.
Psoriasis
of nails can manifest as pitting of nail plate, subungual keratosis, crumbling
of nail plates and onycholysis. Yellowish discoloration, ridges, grooves
and splinter hemorrhages may also occur.
In addition to annular migrans that occur on tongue and cheek in GPP, scaly well-defined papules may occur on glans penis.
Arthritis
may occur in 5-10% of psoriatics. HLA studies revealed that B23, DR3, A26
and B38 are significantly associated with psoriatic arthritis. It is customary
to divide psoriatic arthritis into classic type, rheumatoid type, mutilating
type, oligoarticular type and psoriatic spondylitis.
vTopical
Therapy Other Than Steroids
Contributed
by Dr.Smruti, Sharjah
A.
Tar Therapy:
Tar
has been used in topical therapy for more than a century. It is assumed
to have an antimitotic effect.
Types
of Tar:
Coal tar, wool tar and pine tar. The cruder the tar extract, the more effective
it is. Coal tar is a mixture of thousands of substances produced by primary
condensation during the carbonization of coal; while pine tar is oil from
cade (birch tree).
Concentration
of crude coal tar upto 10% are incorporatedin
various vehicles for local treatment of psoriasis.
Adverse
reactions:
1.
Staining and odour of the tar, lessened in newer preparations
2.
Folliculitis (Commonest)
3.Primary
irritant reaction if used in areas like face, genitalia and flexures.
4.
Carcinogenecity: In cases of prolonged usage with UV light therapy.
Contraindications:
1.
Erythrodermic Psoriasis
2.
Generalized Pustular Psoriasis
3.
Pre-existing folliculitis/ severe acne
B.
Dithranol/Anthralin:
It
is a synthetic derivative of chrysarobin, a tree bark extract. Since it
is an unstable product, combining with salicylic acid stabilizes it.
Dithranol
paste is of unquestionable effectiveness but is highly irritant especially
on the head and neck areas and stains linen irreversibly. Kinetic studies
showing penetration of full epidermis in 100 minutes or less have encouraged
the notion of short contact therapy, which is effective and less irritant.
A concentration of 0.05-0.5% is applied for 10 minutes to one hour under
occlusion.
C.
Salicylic Acid:
It
is a keratolytic agent. It is used in a concentration of 3-5% incorporated
into cold cream or hydrophilic ointment.
D.
UV Light:
Artificial
UV light B is frequently used. In recurring cases, patient may be advised
to own an ultraviolet lamp and expose himself daily to it. A fixed treatment
distance of about 3 feet should be used and time of exposure gradually
increased by a few seconds daily starting with 2 minutes.
Tar
applications or baths prior to UVB have been credited with enhancing its
effect.
For
widespread and recalcitrant psoriasis, ultraviolet therapy combined with
tar or anthralin is the basis for Goeckerman and Ingram regimens.
Goeckerman:
-
2-5% tar preparation is applied daily several times and a tar bath is taken
daily. Excess tar is removed with mineral oil and UV light exposure is
done.
Ingram:-
Daily a coal tar bath in a solution of 120 ml liquor carbonis detergens
to 80 liters of water is followedby
exposure to ultraviolet light for daily increasing periods. An anthralin
paste is then applied to each plaque. Talcum powder is sprinkled over the
lesions and stockinet dressings applied.
E.Iodochlor
hydroxyquine (vioform):
It
has been used frequently in a formula of 3% ointment/cream.
F.
Retinoic Acid as 0.5% ointment base:
It induces a moderately severe reaction at local site and is contraindicated
in generalized psoriasis.
G.
Vitamin D3 (Calcipotriol):
1a,
24-dihidroxy vit D3, a synthetic analogue of 1a,
25 dihydroxy vit D3 (calcitriol)
Mechanism
of action is through induction of terminal differentiation of keratinocytes
and inhibition of T cell proliferation.
It
is widely used in chronic, plaque psoriasis alone or in combination with
potent steroids. It is available as 50mg/gm.
Weekly dosage should not exceed 100gms per week, after which serum calcium
levels increase.
A
drug under trial is maxacalcitol, which is 1a,
25 dihydroxy 22 oxacalcitriol which displays approximately 10 times greater
efficacy at suppressing keratinocyte proliferation in vitro than calcipotriol.
It is being used as 25mg/gm.
Contributed
by Dr.SMS Pillai,Dubai
Topical
steroids are the most widely used medications for psoriasis. They are effective,
convenient to use and affordable.
Corticosteroid
ointments are greasy and messy, but are more effective than cream.
Most
common side effect is cutaneous atrophy. But the atrophy is reversible
in most cases if medication is discontinued early. Other side effects are
telangiectasia, folliculitis, perioral dermatitis etc.
Many
dermatologists believe that tachyphylaxis and steroid rebound are major
limitations of long-term therapy with steroids in psoriasis.
In
the absence of any maintenance therapy, the relapse is estimated to occur
in 60% of cases within one month and 93% of patients in one year. Even
with maintenance corticosteroid therapy, relapse is estimated to occur
in 51% of patients within one month and 71% of patients within 1 year.
Application
of clobetasol propionate 0.05% ointment has been shown to cause a rapid
and statistically significant reduction of plasma cortisol levels within
24 hours. Suppression of HPA axis is indeed the most serious adverse effect
of treatment with super potent steroids. Hence a pulse therapy is advisable
when such topical therapy is attempted.
Contributed
by Dr.Bindu, Sharjah
In
1951,amethopterin (or methotrexate as it is more commonly known), a folic
acid antagonist, was found to be excellent in the control of psoriasis.
20 years later, FDA approved it in psoriasis.
Methotrexate
is structurally similar to folic acid and is a potent inhibitor of the
enzyme dihydrofolate. It binds to it within 60 minutes competitively and
irreversibly, preventing the conversion of dihydrofolate to tetrahydrofolate,
which is necessary for the DNA and RNA synthesis. It acts on 's' phase
of cell cycle.2 agents can reverse the actions of methotrexate, viz leucovorin
and thymidine and can be used in toxicity.
Methotrexate
can be administered oral/IV/IM. Concurrent food intake, especially milk
products may reduce bioavailability in oral dosage.
A
methotrexate candidate should have a debilitating state that either is
uncontrolled by more conventional methods or is not amenable to such therapies.
Contraindications:
Absolute:
Pregnancy, Lactation
Relative:
Decreased renal function, hepatic disease, severe hematological abnormalities,
alcoholism, child bearing age (12weeks before conception: should be stopped
in both sexes), active infectious diseases, h/o potentially serious infection
that could be reactivated, immunodeficiency syndromes, unreliable patient.
Monitoring
Guidelines:
Baseline:
Careful history and physical examination, identification of patients with
increased risk of toxicity, recording concomitant medication to rule out
drug interactions eg, salicylates, NSAID, sulfa, tetracycline, chloramphenicol,
phenytoin, phenothiazines, probenicid, dipyridamole.
Follow-up:
CBC, Platelet, LFT- every week for 4 weeks, 7 days after each dose escalation
CBC,
Platelet, LFT- every 3-4 months after dosage stabilization.
Liver
Biopsy: after every 1.5-2.0 gm total dose for low risk patients.
After
every 1.0 gm total dose for high risk patients
After
every 6 months for IIIA liver changes.
Well,
now liver biopsy is outdated as blood analysis of amino terminal propeptide
of type 3 procollagen is sufficient for evaluation of LF.
Therapeutic
Guidelines:
Occasional
IM if nausea from oral dose.
Oral
dose: single, or more commonly 3 divided doses at 8 am, 8 pm, 8 am once
a week (Rationale: Presumed cell kinetics in psoriasis cell cycle shortened
from 19 days in normal to 37.5 hours in psoriatic epidermis.)
Initial
dose-5-10 mg stat: CBC, LFT after 7 days.
If
Okay, escalate dose to 2.5-5mg per week to get reasonable benefit without
toxicity.
10-12.5
mg/week on an average gives maximum benefit.
IM:
0.2-0.4mg/kg every 7-14 days
Adverse
Effects:
Hepatotoxicity:
Regular monitoring to detect
Pulmonary
Toxicity: Pneumonitis, Pulmonary Fibrosis
Hematological
Effects: Myelosupression
Gastrointestinal:
Nausea, diarrhoea, ulcerative stomatitis, anorexia, vomiting
Potent
Teratogen
Renal
Toxicity only in high dosage
Other:
alopecia, fatigue, phototoxicity, headache, and dizziness.
Contributed
by Dr.M.J.Cyriac, Dubai
Retinoids
are synthetic or natural analogues of vitamin A.
The
3 main ones are:
1.
Isotretinoin (13 cis retinoic acid)
2.
Etretinate
3.
Acitretin
Acitretin
is an active metabolite of Etretinate. Etretinate is an ester and acitretin
a corresponding free acid. Its great advantage over etretinate is its decreased
lipophilicity, which results in elimination half-life of 50 hours as opposed
to more than 80 days for etretinate. However the clinical efficacy and
side effects are similar to etretinate.
The
mode of action of retinoids is not fully established. It seems to induce
a better maturation in keratinocytes and to reduce the neutrophil chemo
taxis in pustular psoriasis.
Indications:
1.
Generalized Pustular Psoriasis: Considered to be the drug of choice.
2.
Psoriatic erythroderma.
3.Severe
psoriasis vulgaris, where other modalities have either failed or are contraindicated.
4.Palmo-plantar
pustular psoriasis.
Dose:
0.5-1
mg/kg/day is the usual initial dose of etretinate. Maintenance dose of
0.5 to 0.75mg/kg/day. Remission may take anywhere from 12-24 weeks. Relapses
are very common following discontinuation of treatment.
Acitretin-
an optimum dose of 50mg daily (mean 0.66mg/kg/day) is recommended.
Contraindications:
1.Women
of child bearing age, unless the psoriasis is unresponsive to other therapies
or where clinical condition contraindicates the use of other regimens.
In
such cases the following precautions are to be strictly adhered to:
a.
Has received both oral and written warning of hazards of taking acitretin
b.
Should be on reliable form of contraception
c.
Should have negative serum and urine pregnancy test done at least 1 week
prior to beginning treatment.
d.
Treatment should be started on the 2nd or 3rd day of next normal menstrual
period.
2.
Pregnancy
3.
Children
4.
Active liver disease
5.
Pre-existing hyperlipidemia
Side
Effects:
-
Almost 99% of patients receiving retinoids develop some sort of side effect.
-
It is highly teratogenic.
-
The retinoids are lipophilic and are retained in the body for a considerably
longer period of time. Sowomen
receiving the drug should avoid pregnancy for a period of 3 years.
-
It does not have any significant efect on the semen.
-
Lipid abnormalities in the form of increased serum triglycerides and cholesterol
may necessitate discontinuation of therapy. In mild cases, the abnormality
may be alleviated by concomitant administration of fish oils.
-
Liver enzyme elevation, hepatitis and jaundice
-
Radiological spinal changes including anterior spinal ligament calcification,
osteophytes, disc abnormality, DISH (diffuse idiopathic skeletal hyperosteosis)
can occur
-
In children, premature closure of epiphyses, growth retardation andhyperosteosis
can occur
-
Dryness of the lip, nose, mouth, eyes, throat with peeling of skin, exfoliative
cheilitis, uveitis, balanitis, gingivitis, corneal ulceration, burning
sensation of skin, atrophy of skin, alopecia, epistaxis, increased bruising,
generalized erythema
-
Purulent paronychia may necessitate stopping of therapy.
-
Pseudotumour cerebri is not uncommon
Drug
Interactions:
1.
Do not give tetracyclines along with retinoids (pseudotumour cerebri)
2.
No supplementation with vitamin A
3.Concommitant
methotrexate increases hepatotoxicity
4.
Ethanol should not be given along with acitretin because it is converted
to etretin
Contributed
by Dr. Sathish Kumar, Dubai
Parrish
et al first reported this mode of therapy in 1974.
It consists of ingestion of Psoralen in the dose of 0.6-mg/kg body weight
on alternate days and followed in 2-3 hours later by UV radiation for graded
periods.
The
commonly used psoralens are 8-methoxy psoralen and 4,5,8 trimethoxy psoralen.
PUVA
therapy
affects DNA synthesis and proliferation of cells in psoriatics by 2 mechanisms:
a.
An anoxic reaction that affects cellular DNA with the formation of photo
adducts.
b.
An oxygen dependent reaction where free radicals and reactive oxygen formed
may damage the membrane of lipid per oxidation and induce activation of
mediators of the eicosanoid system.
PUVA
therapy
also reduces the chemo tactic activity of the psoriatic leukotactic factor.
Topical
PUVA has been tried in the form of PUVA bath. Trimethoxy psoralen 50mg
in 100ml ethanol is added to a 150-litre bath. Patient is allowed to bath
for 15 minutes and then exposed to UVA at 290-320 nm. Photosensitivity
is achieved immediately after this bath is 15 times greater than after
oral psoralen and side effects like nausea, headache can be minimized by
PUVA bath.
Side
effects of PUVA therapy:
-
Nausea, vomiting, headache, vertigo, erythema, pruritus, blistering
-
Koebner phenomenon
-
Hypertrichosis, hyper pigmentation
-
Lichenoid eruption
-
Photo-onycholysis
-
Premature ageing of skin, Cataract formation
-
Increased incidence of skin cancers etc.
Taking
steps to minimize the total dose of PUVA, by combination therapy with topical
PUVA, oral retinoids and methotrexate, can reduce these side effects.
vOther
Immunosuppressive Therapy
Contributed
by Dr.S.M.S.Pillai, Dubai
Cyclosporine
(Cy A)
is a cyclic undecapeptide derived from fungus Toylypocladium inflatum gams.
It is indicated for the treatment of adult non immuno-compromised patients
with severe recalcitrant psoriasis who have failed to respond to at least
one systemic therapy or in patients for whom other systemic therapies are
contraindicated or cannot be tolerated.
To
start with it is given in the dose of 3 mg/Kg body weight in two divided
doses, which can be gradually increased to 5mg/Kg/day depending upon the
therapeutic response. The effects of Cy A are evident within weeks; they
are dose dependent.
The
exact mechanism by which Cy A acts in psoriasis is not clear. It possibly
down modulates proinflammatory cytokines that are increased in psoriatic
lesions
Cy
A is contraindicated in renal diseases, past or present malignancy, and
uncontrolled hypertension. It is not safe for pregnant women and during
lactation. Adverse effects include hypertension with raised serum creatinine
level, IT comlicationss, hirsutism, headache and haemorrhagic gingivitis.
TACROLIMUS
a macrolide immunosuppressive isolated from streptomyces tsukubaensis act
by inhibiting the keratonocyte receptor pathway, an endogenous regulator
of the cell cycle. Topical application of the drug is promising in the
initial pilot studies.
ASCOMYCIN
another immunosuppressant macrolide is effective in the concentration of
0.1 to 0.5%.
OTHER
drugs used and tried are TYROSINE KINASE INHIBITORS, ZIDOVUDINE, AURANOFIN,
and SULFASALAZINE.